Valid West Virginia Do Not Resuscitate Order Document
Key takeaways
When filling out and using the West Virginia Do Not Resuscitate Order form, it is essential to keep a few important points in mind.
- Understand the Purpose: This form is designed to communicate a patient’s wishes regarding resuscitation efforts in case of a medical emergency.
- Eligibility: Only patients who are 18 years or older, or their legal representatives, can complete this form.
- Signature Requirement: The form must be signed by the patient or their authorized representative, along with a physician’s signature to be valid.
- Accessibility: Once completed, keep the form in an easily accessible location, and share copies with healthcare providers and family members.
By following these key takeaways, you can ensure that the Do Not Resuscitate Order accurately reflects your or your loved one's wishes and is properly recognized by medical personnel.
Other Common West Virginia Templates
Notary Acknowledgement Sample - Each state has its own requirements for the Notary Acknowledgment, so checking local laws is crucial.
When completing the sale of an ATV, it is essential to utilize the New York ATV Bill of Sale form, which can be found on smarttemplates.net. This form ensures that all necessary details regarding the sale and transfer are properly documented, providing a clear record for both the buyer and the seller.
How to Get Power of Attorney in Wv - This form enables an individual to appoint someone to make decisions regarding finances or health care.
Wv Living Will - The form outlines specific medical treatments to accept or refuse in case of incapacitation.
Misconceptions
Understanding the West Virginia Do Not Resuscitate (DNR) Order form is crucial for making informed healthcare decisions. However, several misconceptions can lead to confusion. Here are eight common misunderstandings about the DNR form:
- A DNR means no medical care at all. Many people believe that a DNR order implies that no medical treatment will be provided. In reality, a DNR only applies to resuscitation efforts in the event of cardiac arrest. Other medical treatments will still be administered as needed.
- A DNR is only for terminally ill patients. While DNR orders are often associated with terminal illnesses, they can be appropriate for anyone who wishes to avoid resuscitation in specific circumstances, regardless of their overall health status.
- A DNR is permanent and cannot be changed. Some individuals think that once a DNR is signed, it cannot be altered. In fact, a DNR can be revoked or modified at any time by the patient or their legal representative.
- Having a DNR means you cannot receive palliative care. This is a common myth. Palliative care focuses on comfort and quality of life, and it can be provided alongside a DNR order.
- All healthcare providers recognize the DNR order. While most providers honor DNR orders, it is essential to ensure that your DNR is properly documented and communicated to all healthcare professionals involved in your care.
- A DNR must be signed in front of witnesses. In West Virginia, a DNR order does not require witnesses for it to be valid. However, it must be signed by a physician and the patient or their authorized representative.
- You can only have a DNR if you are in a hospital. A DNR order can be established outside of a hospital setting. It is important to discuss your wishes with your healthcare provider and ensure that the order is documented appropriately.
- People with DNR orders are treated differently by healthcare providers. Some believe that having a DNR will lead to less attentive care. In reality, healthcare providers are committed to providing appropriate care regardless of a patient's resuscitation preferences.
Understanding these misconceptions can help individuals make informed decisions about their healthcare and ensure that their wishes are respected.
Similar forms
The West Virginia Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive. An Advance Directive is a legal document that outlines a person's preferences for medical treatment in situations where they cannot communicate their wishes. Like the DNR, it allows individuals to express their desires regarding life-sustaining treatments. Both documents ensure that a person's healthcare choices are respected, providing peace of mind to both the individual and their loved ones during critical medical situations.
Another document similar to the DNR is the Medical Power of Attorney. This legal instrument designates a specific person to make healthcare decisions on behalf of someone else if they become incapacitated. While the DNR focuses on the specific wish to forgo resuscitation, the Medical Power of Attorney allows for broader decision-making. Both documents emphasize the importance of personal choice in medical care and ensure that a person's values and preferences are honored even when they cannot speak for themselves.
The Living Will is another document that aligns closely with the DNR Order. A Living Will explicitly states an individual's wishes regarding medical treatment in situations where they are terminally ill or permanently unconscious. Like the DNR, it serves as a guide for healthcare providers and family members, clarifying what types of life-sustaining measures should or should not be taken. Both documents empower individuals to take control of their healthcare decisions and alleviate the burden of making difficult choices for loved ones.
The Physician Orders for Life-Sustaining Treatment (POLST) form is also similar to the DNR Order. The POLST is a medical order that translates a patient's preferences regarding life-sustaining treatments into actionable medical directives. It is often used for patients with serious illnesses and serves as a more detailed version of a DNR. Both documents aim to ensure that healthcare providers understand and respect a patient's wishes, providing clear guidance during emergencies.
Another relevant document is the Comfort Care Order. This form is designed to prioritize comfort and quality of life for patients who are nearing the end of life. While a DNR specifically addresses resuscitation efforts, a Comfort Care Order focuses on alleviating pain and discomfort without aggressive medical interventions. Both documents reflect a compassionate approach to healthcare, emphasizing the importance of dignity and comfort in the final stages of life.
Understanding the various healthcare documents available can significantly impact the quality of care a person receives. For instance, similar to the Medical Power of Attorney, a POA provides individuals with the ability to designate a trusted person to make critical decisions on their behalf when they are unable to do so, ensuring that their healthcare choices are honored in accordance with their values and wishes.
Lastly, the Do Not Intubate (DNI) Order is akin to the DNR Order. A DNI specifically instructs healthcare providers not to insert a breathing tube if a patient cannot breathe on their own. Like the DNR, it is a clear expression of a patient's wishes regarding life-sustaining measures. Both documents are vital tools for individuals who want to ensure their preferences are honored, particularly in critical situations where every second counts.
Key Facts about West Virginia Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order in West Virginia?
A Do Not Resuscitate Order is a legal document that informs medical personnel not to perform cardiopulmonary resuscitation (CPR) or other life-saving measures if a patient’s heart stops beating or they stop breathing. In West Virginia, this order is intended to respect the wishes of individuals who do not wish to receive such interventions in the event of a medical emergency.
Who can complete a DNR Order in West Virginia?
In West Virginia, a DNR Order can be completed by a patient who is at least 18 years old and has the capacity to make medical decisions. If the patient is unable to make decisions, a legally authorized representative, such as a family member or a healthcare proxy, may complete the order on their behalf.
How do I obtain a DNR Order form in West Virginia?
You can obtain a DNR Order form from various sources, including healthcare providers, hospitals, and online resources. The West Virginia Department of Health and Human Resources provides a standardized DNR form that can be downloaded and printed for use.
What information is required on the DNR Order form?
The DNR Order form typically requires the patient's name, date of birth, and a clear statement of the individual's wishes regarding resuscitation. Additionally, the form must be signed by the patient or their authorized representative and a physician to be considered valid.
Is a DNR Order valid in all healthcare settings?
Yes, once properly completed and signed, a DNR Order is valid in all healthcare settings in West Virginia. This includes hospitals, nursing homes, and even at home, as long as the form is readily available to medical personnel when needed.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time by the patient or their authorized representative. To revoke the order, the individual should inform their healthcare provider and destroy any copies of the DNR form. It is essential to ensure that all relevant parties are aware of the revocation.
What should I do if I have a DNR Order?
If you have a DNR Order, it is crucial to keep it in an accessible place, such as on your refrigerator or with your medical records. Inform family members, friends, and healthcare providers about your DNR wishes to ensure they are honored during a medical emergency.
Are there any specific requirements for the signature on the DNR Order?
The DNR Order must be signed by the patient or their authorized representative and must also include the signature of a physician. The physician's signature confirms that the patient has been informed about the implications of the DNR Order and that it reflects the patient's wishes.
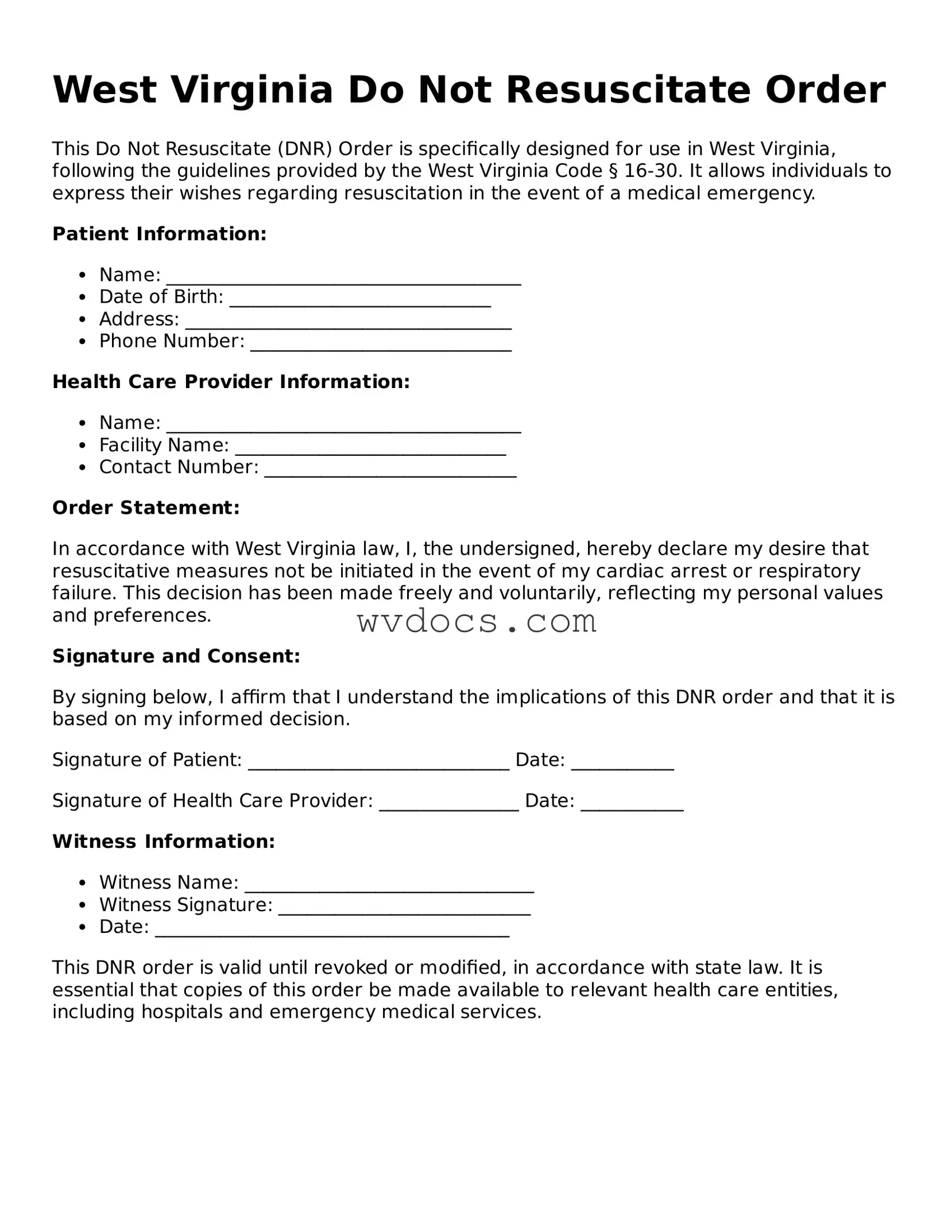
Preview - West Virginia Do Not Resuscitate Order Form
West Virginia Do Not Resuscitate Order
This Do Not Resuscitate (DNR) Order is specifically designed for use in West Virginia, following the guidelines provided by the West Virginia Code § 16-30. It allows individuals to express their wishes regarding resuscitation in the event of a medical emergency.
Patient Information:
- Name: ______________________________________
- Date of Birth: ____________________________
- Address: ___________________________________
- Phone Number: ____________________________
Health Care Provider Information:
- Name: ______________________________________
- Facility Name: _____________________________
- Contact Number: ___________________________
Order Statement:
In accordance with West Virginia law, I, the undersigned, hereby declare my desire that resuscitative measures not be initiated in the event of my cardiac arrest or respiratory failure. This decision has been made freely and voluntarily, reflecting my personal values and preferences.
Signature and Consent:
By signing below, I affirm that I understand the implications of this DNR order and that it is based on my informed decision.
Signature of Patient: ____________________________ Date: ___________
Signature of Health Care Provider: _______________ Date: ___________
Witness Information:
- Witness Name: _______________________________
- Witness Signature: ___________________________
- Date: ______________________________________
This DNR order is valid until revoked or modified, in accordance with state law. It is essential that copies of this order be made available to relevant health care entities, including hospitals and emergency medical services.
Documents used along the form
The West Virginia Do Not Resuscitate (DNR) Order form serves as a critical document for individuals wishing to outline their preferences regarding resuscitation efforts in medical emergencies. However, several other forms and documents often accompany the DNR to ensure comprehensive healthcare planning and decision-making. Below is a list of these related documents, each playing a vital role in the overall process.
- Advance Directive: This document allows individuals to specify their healthcare preferences in advance, including decisions about life-sustaining treatments and appointing a healthcare proxy.
- Healthcare Power of Attorney: A legal document that designates a specific person to make medical decisions on behalf of an individual if they become unable to do so themselves.
- Living Will: This form outlines an individual’s wishes regarding medical treatment in situations where they cannot communicate their preferences, particularly concerning end-of-life care.
- Physician Orders for Life-Sustaining Treatment (POLST): A medical order that translates an individual’s wishes regarding treatment into actionable orders for healthcare providers, ensuring that preferences are honored during emergencies.
- Do Not Hospitalize Order: This document expresses a patient’s desire to avoid hospitalization under certain circumstances, often used in conjunction with a DNR order.
- Medical History Form: A comprehensive overview of a patient’s medical background, including past illnesses, surgeries, and medications, which can inform treatment decisions.
- Medication List: A detailed list of all medications a patient is currently taking, which is crucial for ensuring safe and effective medical care.
- ATV Bill of Sale: Essential for transferring ownership of an all-terrain vehicle, the ATV Bill of Sale form serves as proof of transaction and is necessary for tax and registration purposes.
- Emergency Contact Information: A document that provides contact details for family members or friends who should be reached in case of a medical emergency.
These documents collectively enhance the clarity of an individual's healthcare preferences and ensure that medical professionals have the necessary information to honor those wishes. Properly completed, they can provide peace of mind for both patients and their loved ones, facilitating informed decision-making during critical moments.